Pulpitis is an inflammation of the tooth pulp caused by cavities (in 80% of cases), trauma, or iatrogenic factors. Symptoms: sharp pain, sensitivity to temperature, and darkening of the enamel. Diagnosis: clinical exam, X-ray, and 3D tomography. Treatment: conservative or endodontic, often using microscopes and lasers. In children, the focus is on preserving baby teeth. Prevention: proper oral hygiene and regular check-ups. At Gallant, we guarantee high-quality treatment!
Pulpitis: what it is, symptoms, diagnosis, and modern treatment approaches
Sometimes, cavities develop without any visible symptoms. A person may feel no pain and therefore doesn’t rush to the dentist. In such cases, it’s easy to miss the early stage of the disease — meanwhile, the infection continues to spread deeper into the tooth. This is how pulpitis begins.
It’s one of the most common reasons people seek dental care. Nearly every fifth appointment at Gallant Dental Clinic in Korsun and Horodyshche is related to this condition. Fortunately, modern dentistry allows us to treat pulpitis at various stages. Still, the earlier the problem is diagnosed, the higher the chance of saving the tooth and avoiding complications.
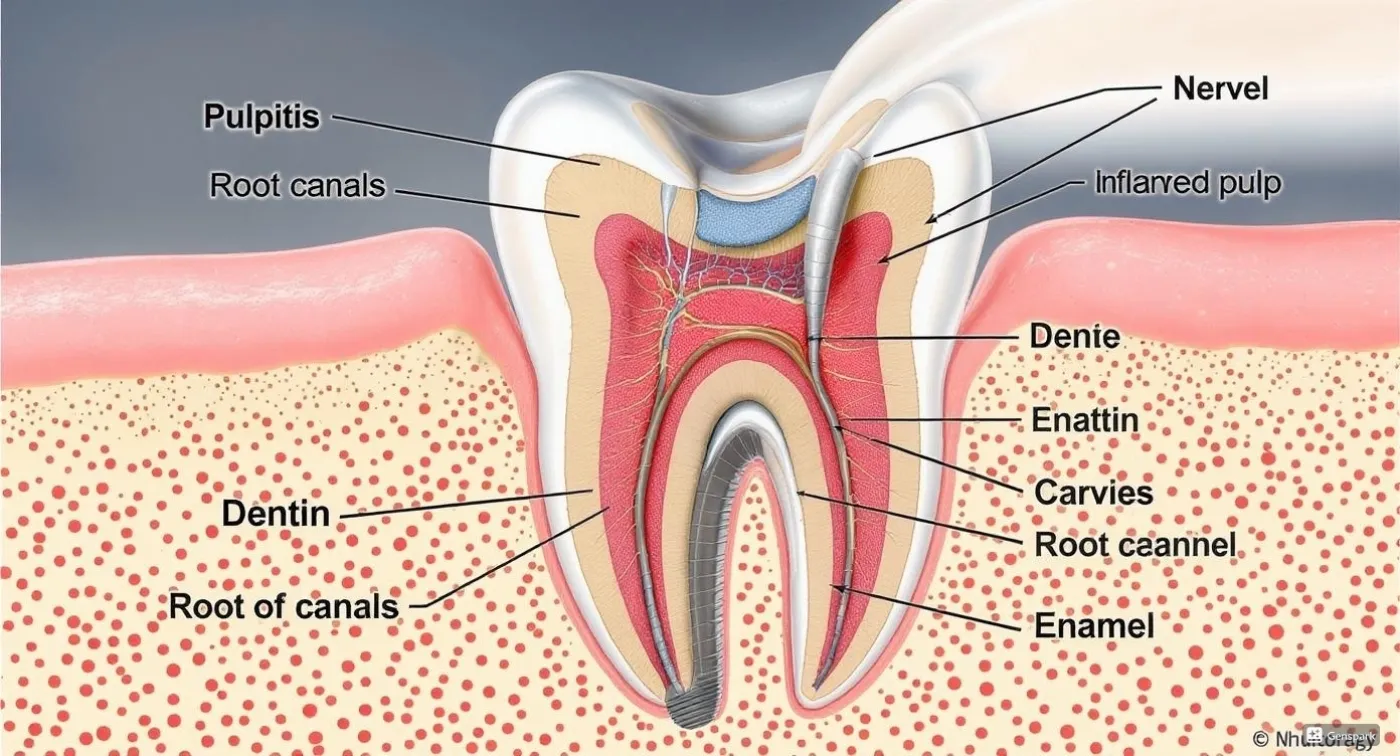
What is dental pulpitis: anatomy and function of the pulp
Pulpitis is the inflammation of the tooth pulp. It is the soft tissue beneath the enamel and dentin that contains a rich network of blood vessels and nerve endings. It supplies the hard tissues of the tooth with nutrients.
Main causes of pulpitis: from cavities to trauma
When it comes to pulpitis, its causes are usually divided into three main groups:
- Infectious (most common) - untreated deep cavities (in 80% of cases), secondary caries under a filling, or infection spreading from the gums (periodontogenic infection).
- Non-infectious - trauma from impact, cracks in the tooth, or other mechanical damage, as well as thermal or chemical exposure that injures the pulp and triggers inflammation.
- Iatrogenic - improper cavity treatment (e.g., overheating during drilling or incomplete removal of decayed tissue).
Classification of Pulpitis: Types and Forms of the Disease
Pulpitis can be classified based on several factors: the course of the disease, the nature of inflammation, clinical symptoms, and morphological changes in the tissue.
Based on the course of the disease, the main forms of pulpitis include:
- Acute pulpitis, which is further divided into: focal (serous) - the initial stage of inflammation, characterised by moderate pain; diffuse - the inflammation spreads throughout the pulp, and the pain intensifies; purulent - accompanied by exudate formation and severe pain.
- Chronic pulpitis, which usually develops as a complication of untreated acute pulpitis. It includes: fibrous - fibrous tissue grows and forms scars; the pain is mild, but the tooth is sensitive to temperature; gangrenous - the pulp dies, causing bad breath and possible fistula formation; hypertrophic - the pulp enlarges and grows into the carious cavity.
Other less common types include concretional pulpitis - calcifications (pulp stones) form inside the pulp; and retrograde pulpitis - involves damage to the tooth nerve and jawbone tissue.
When symptoms return after a period of remission, this is considered an exacerbation of chronic pulpitis.
Symptoms of Pulpitis: How to Recognise the Condition
The general symptoms of pulpitis depend on the form and stage of the inflammatory process. The main symptom of the acute form is spontaneous pain that becomes more intense at night.
The affected tooth responds to temperature stimuli. Pain may radiate to neighbouring teeth, the ear, or the temple.
Typical symptoms of chronic pulpitis include:
- Mild pain with periodic flare-ups;
- Unpleasant odour from the mouth;
- Darkening or greyish discolouration of the enamel.
At the same time, it is important to be able to distinguish different types of pulpitis from other dental conditions. For example, with tooth decay, the tooth hurts when irritated (e.g. by cold or sweet); with periodontitis, pain occurs when pressure is applied to the tooth; with trigeminal neuralgia, the pain is sharp, shooting, intense but short-lived - while the pain caused by pulpitis is typically dull, throbbing, and gradually intensifies.
Modern Diagnosis of Pulpitis: Methods and Approaches
When pulpitis is suspected, diagnosis begins with taking the patient's medical history and performing a traditional dental examination. Additional diagnostic tools may include a thermal test (to evaluate the tooth’s reaction to hot and cold), electroodontodiagnostics to assess the condition of the pulp, X-ray imaging or digital radiovisiography to examine the root canal system.
More advanced and precise diagnostic methods are gaining popularity thanks to modern technologies. These include 3D tomography, transillumination, laser Doppler flowmetry, optical coherence tomography, and others.
Modern Approaches to Pulpitis Treatment
The method of pulpitis treatment depends on the type and stage of the inflammatory process.
Conservative treatment focuses on preserving the vitality of the pulp. This may include biological techniques (applicable when tissue damage is minimal), direct or indirect pulp capping, or partial pulpotomy (removal of the affected part of the pulp tissue). When the tissue is extensively damaged or necrotic, surgical methods involving full pulp removal are used. Endodontic treatment involves thorough cleaning and sealing of the root canals. Increasingly, advanced technologies are applied to treat both acute and chronic forms of pulpitis. These include operating microscopes, endodontic motors, lasers, and ultrasound systems.
The combination of classic and modern techniques enables fast, effective, and painless treatment of even complex cases while preserving the tooth.
Pulpitis in Children: Diagnostic and Treatment Features
Due to the specifics of the inflammatory process in primary teeth, treating pulpitis in children has its own peculiarities. In baby teeth, the dentin walls are quite thin and the pulp chambers are relatively large. This facilitates rapid spread of infection and swift disease progression, often without pronounced symptoms. Treatment of pulpitis in children focuses on preserving the primary tooth until its natural replacement. Depending on the stage of the disease, treatment may involve pulp-preserving methods or complete pulp removal.
When treating permanent teeth in children, it is essential to consider that root formation is still ongoing. In such cases, treatment strategies aim to preserve the root growth zone, support natural development, and promote tissue regeneration. This approach known as regenerative endodontics.
Complications of Pulpitis and Their Prevention
Pulpitis complications can arise from various causes and present in different forms. If left untreated, the inflammation may lead to pulp necrosis, periodontitis, abscesses, phlegmon, or osteomyelitis - all involving purulent processes and destruction of soft or bone tissue in the jaw.
Complications may also occur after treatment. Some are considered normal, such as postoperative discomfort. Others may result from medical errors or unforeseen issues during treatment, such as root perforation, instrument fracture, or overfilling of the root canal beyond its apex.
Timely dental visits, high-quality canal cleaning, and the use of reliable sealing materials significantly increase the chances that a treated tooth will remain functional for decades — provided that the patient maintains proper oral hygiene, undergoes regular professional cleanings, and treats any new carious lesions promptly.
Pulpitis Prevention: How to Avoid the Disease
Preventing pulpitis is easier and far more effective than treating it. The key to avoiding pulp inflammation lies in maintaining good oral hygiene, regular dental check-ups, timely treatment of cavities, and a balanced diet. High-quality dental fillings are essential in preventing pulpitis. The outcomes of treatment should be monitored through routine follow-up visits and X-ray imaging to detect potential problems early.
First Aid for Suspected Pulpitis
There are no home remedies or over-the-counter medications that can cure pulpitis. However, while waiting to see a dentist, pain can be temporarily managed by taking an analgesic, such as ibuprofen or paracetamol. It is important to follow the dosage instructions and check for any contraindications before use. Keep in mind that such pain relief is only a short-term solution.
To ease discomfort, you can rinse your mouth with a saltwater solution or an alcohol-free antiseptic. Cold compresses applied externally to the cheek may help reduce inflammation and numb the pain. However, applying heat is strictly prohibited, as it may worsen the inflammation.
It is crucial not to delay a visit to the dentist once pain appears. Self-treatment will not resolve the issue — it may only increase the risk of serious complications. Seek urgent medical attention if the pain persists despite taking painkillers, if there is swelling, fever, or if the tooth becomes extremely sensitive to touch.
Rehabilitation After Pulpitis Treatment
Following endodontic treatment, it's important to avoid putting stress on the treated tooth for several days - refrain from eating hard, very cold, or very hot foods.
After pulpitis treatment, the tooth needs to be restored to its original shape. Depending on the extent of damage, this may require a filling, inlay, or crown.
Treatment may last from one to several appointments, depending on the complexity of the case. In the months following the procedure, typically within 6 months, a follow-up X-ray is recommended to assess the condition of the root canals and surrounding tissues.
Conclusion: A Modern Approach to Pulpitis Treatment
Advanced diagnostic tools and modern treatment methods for pulpitis make it possible to preserve the tooth and prevent complications. The key is not to ignore the early signs of the disease and to undergo regular preventive check-ups with a dentist to catch early stages of cavities or pulp inflammation in time.
Request a call
We will contact you to schedule a convenient time for your consultation and connect you with the right specialist
More articles
We have gathered all the most interesting posts from our specialist doctors in our blog just for you
Dental Treatment During Pregnancy: Myths and Facts

Bruxism (Teeth Grinding) and How to Get Rid of It Forever

Request a call
We’ll get back to you shortly!

Leave a Review
Your feedback means a lot to us!



