Sleep apnea is a condition involving breathing interruptions during sleep, often accompanied by snoring. There are three main types: obstructive, central, and mixed. Causes: anatomical features, obesity, and lifestyle factors. Symptoms: excessive daytime sleepiness, morning headaches, and episodes of gasping or choking during sleep. Diagnosis is typically made using polysomnography (a sleep study). Treatment options: CPAP therapy, oral appliances (sleep mouthguards), and surgical intervention. A dentist can sometimes detect signs of sleep apnea by examining the jaw structure and tooth enamel.

What is sleep apnea: symptoms and modern treatment methods for breathing disorders during sleep
Have you ever tried holding your breath? How long could you manage? Now imagine people who, dozens or even hundreds of times a night, involuntarily stop breathing in their sleep. Each pause can last up to 30 seconds. And there are millions of such people around the world. According to studies, around 20–30% of men and 10% of women suffer from this condition—often without even knowing it.
This disorder is called sleep apnea, and its seriousness is frequently underestimated. In fact, if left untreated, it can lead to severe complications, including sudden death. While many believe that sleep apnea is incurable, modern medicine offers a variety of effective treatments.
What Is Sleep Apnea Syndrome: Medical Definition and Mechanisms
Most people have heard of sleep apnea which is repeated pauses in breathing during sleep, often accompanied by snoring and sudden awakenings. However, snoring and sleep apnea are not the same. The characteristic loud noise is just one potential symptom. Breathing may stop even without snoring.
In addition to apnea (a complete stop in breathing for 10 seconds or more), there is also hypopnea. In this case, breathing doesn’t stop completely, but becomes significantly reduced, causing blood oxygen levels to drop by 3% or more.
To determine the severity of the condition, doctors use a special metric called the Apnea-Hypopnea Index (AHI). It indicates how many times per hour a person stops breathing or breathes very shallowly during sleep: up to 5 events/hour – normal; 5 to 15 events/hour – mild form; 15 to 30 events/hour – moderate; over 30 events/hour – severe form
This condition causes hypoxia (low oxygen in the blood), which is dangerous for the heart, brain, and overall health.
There are several types of sleep apnea:
- Obstructive Sleep Apnea (OSA) – the most common type, caused by blockage of the upper airways
- Central Sleep Apnea – due to disrupted brain signals that control breathing
- Mixed Sleep Apnea – a combination of obstructive and central features
Understanding airway obstruction, neural regulation of breathing, and anatomical factors is crucial for timely diagnosis and effective treatment.
Causes of Sleep Apnea: From Anatomy to Lifestyle
There are various known causes of sleep apnea:
- Anatomical factors – structural features of the upper airways, enlarged tonsils, deviated nasal septum, retrognathia (receded lower jaw), micrognathia (small jaw);
- Physiological factors – obesity, neck circumference over 43 cm in men and over 40 cm in women, genetic predisposition, gender differences (more common in men), and age (risk increases with age);
- External influences – smoking, alcohol consumption, use of sedative medications, body position during sleep (sleeping on the back promotes airway obstruction), stress, and chronic fatigue.
In addition, underlying health conditions may contribute to the development of this disorder. Sleep apnea is often associated with hypothyroidism, acromegaly, heart failure, and neurological diseases.
Symptoms of Sleep Apnea: How to Recognise Breathing Disruption
You might suspect someone has sleep apnea if they exhibit loud, irregular snoring, excessive night sweating, waking up gasping for air, or frequent nighttime urination. A bed partner may notice repeated breathing pauses during the night.
During the day, people with this condition often complain of excessive sleepiness, morning headaches, concentration or memory issues, irritability, mood swings, or reduced libido.
Sleep apnea is also frequently found in individuals with high blood pressure, obesity, enlarged tonsils, or retrognathia.
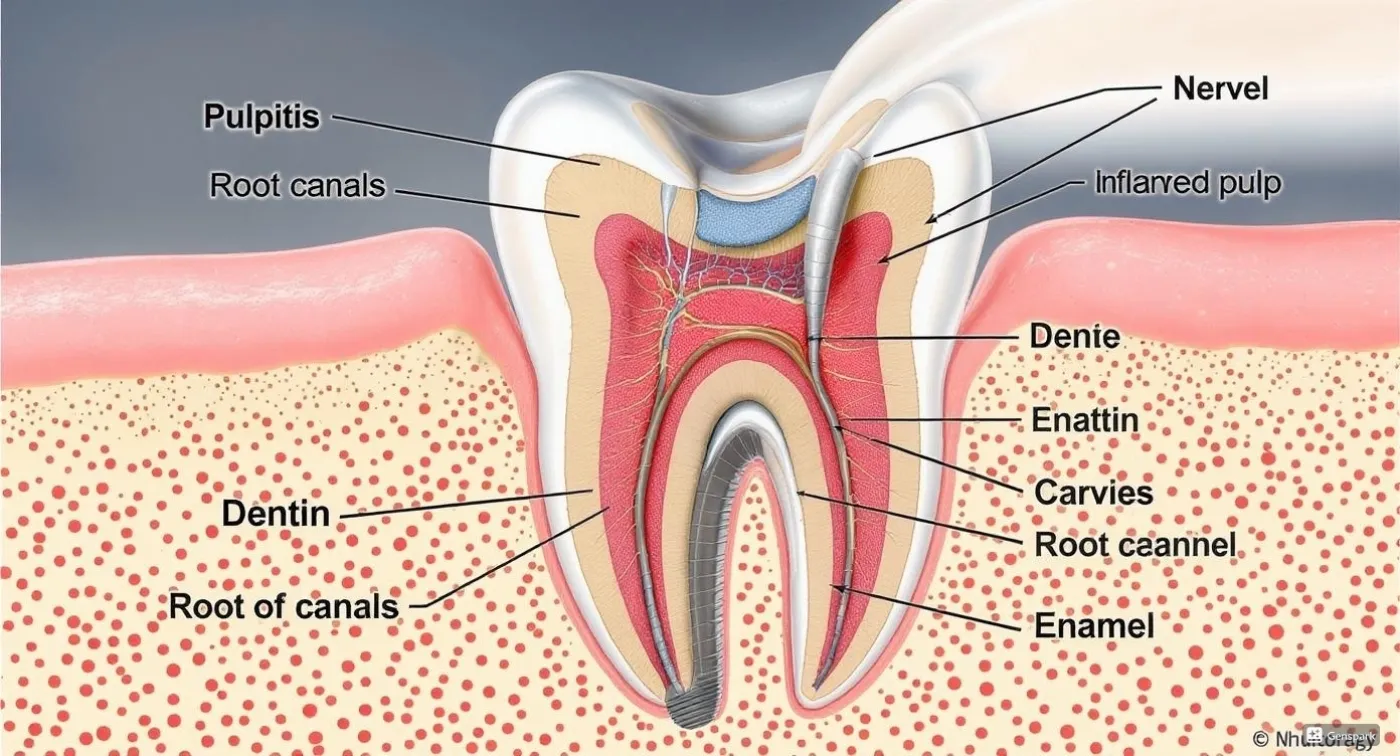
Interestingly, many people first learn they may have sleep apnea during a dental visit. An experienced dentist may suspect the disorder by observing jaw and palate structure or worn-down tooth enamel—the latter often results from nighttime teeth grinding due to oxygen deficiency.
If the condition is not identified and treated in time, it may lead to serious health complications.
Modern Diagnosis of Sleep Apnea: From Screening to Polysomnography
Modern medicine offers precise tools to diagnose sleep apnea through various methods.
Diagnostics begins with an initial assessment and screening. The physician collects the patient’s medical history and complaints, evaluates daytime sleepiness using the Epworth Sleepiness Scale, and performs a physical examination (measuring neck circumference, body mass index). Screening questionnaires such as STOP-BANG or the Berlin Questionnaire also help identify the disorder.
However, one of the most effective diagnostic methods is polysomnography. During the procedure, different sensors are attached to the body to monitor physiological sleep indicators throughout the night: brain activity, heart rate, blood oxygen levels, breathing, body movements, and more. Based on the results, the type of disorder, its severity, and its impact on the body can be determined. By the way, there are home testing devices with similar functions, although their accuracy is inferior to that of polysomnography.
If more detailed examination is required to confirm the diagnosis, comprehensive diagnostics may be used, such as pulse oximetry, respiratory polygraphy, nasal airflow measurement (flowmetry), and nasopharyngeal fibroscopy, among others.
Treatment of Sleep Apnea: From Lifestyle Changes to CPAP Therapy
Among the first-line recommendations for treating apnea is changing one’s lifestyle. This includes weight loss (in cases of excess body weight), establishing a healthy sleep schedule, and giving up smoking and alcohol. Sleeping on one’s side instead of the back also helps prevent breathing interruptions.
A more effective treatment involves the use of CPAP devices. These are machines with a mask that deliver air under pressure to prevent the airways from collapsing during sleep. There are standard devices, automatic Auto-CPAP machines, and bi-level BiPAP machines, allowing for individual selection. It may take time to get used to sleeping with a mask, but the high effectiveness of this method makes it worthwhile.
As a more affordable alternative to CPAP machines, intraoral appliances are also used. These slightly push the lower jaw forward, along with hypoglossal nerve stimulators, positional therapy devices, and nasal dilators. Before using mouthguards or similar tools, it is advisable to consult a dentist. In fact, the dentists at Gallant private clinic have experience working with patients who have apnea. They can help choose a solution that normalises nighttime breathing without harming the teeth.
In particularly severe cases, surgical methods are used to treat sleep apnea, such as uvulopalatopharyngoplasty, septoplasty, tonsillectomy, adenoidectomy, as well as modern minimally invasive surgeries.
CPAP Therapy: A Complete Guide to Use and Adaptation
For CPAP therapy, standard devices can be used (for mild or moderate forms of the disorder), automatic machines (convenient at the start of treatment and for patients with fluctuating indicators), and bi-level devices (provide different pressures during inhalation and exhalation, suitable for severe obstruction). When choosing a model, attention should be paid to the type of mask (nasal, full-face, nasal cannula), as well as the presence of additional features: humidifier, air heating, and more.
Request a call
We will contact you to schedule a convenient time for your consultation and connect you with the right specialist
More articles
We have gathered all the most interesting posts from our specialist doctors in our blog just for you
Dental Treatment During Pregnancy: Myths and Facts

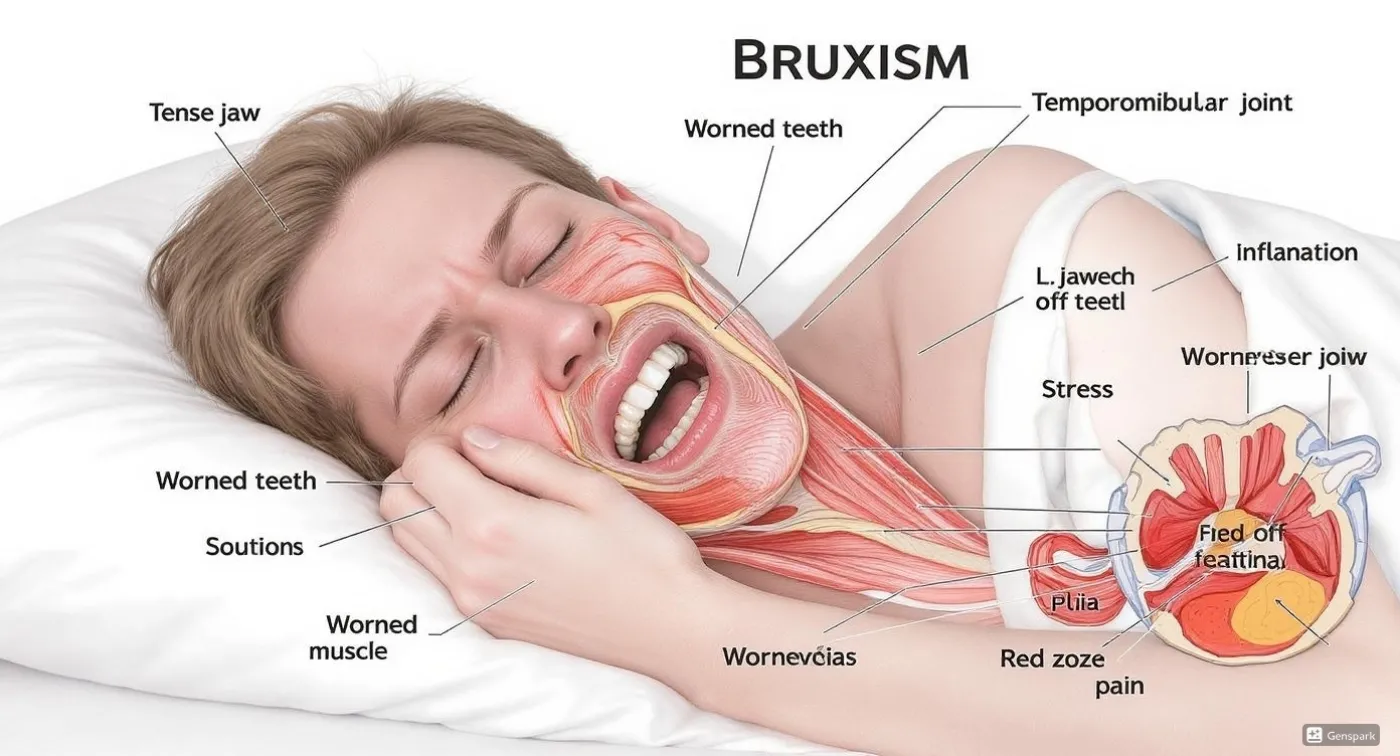
Bruxism (Teeth Grinding) and How to Get Rid of It Forever

Request a call
We’ll get back to you shortly!

Leave a Review
Your feedback means a lot to us!