Periodontitis is more than just a toothache - it’s a serious condition that can lead to systemic complications. Early diagnosis and comprehensive treatment make it possible to save the tooth in 70–90% of cases. The best strategy is prevention through regular check-ups and timely treatment of cavities.

Periodontitis: What Is It, How to Recognise It, and How to Treat It?
Periodontitis is a common dental condition caused by inflammation of the tissues surrounding the tooth root. It often develops as a complication of untreated pulpitis and is accompanied by intense pain, the formation of purulent abscesses, and the risk of serious complications. The infection from the inflammation site can spread throughout the body, affecting the heart, joints, and, in severe cases, even leading to sepsis or osteomyelitis. That’s why early diagnosis and prompt dental care are essential - the sooner treatment begins, the higher the chance of saving the tooth and avoiding complications.
Understanding Periodontitis
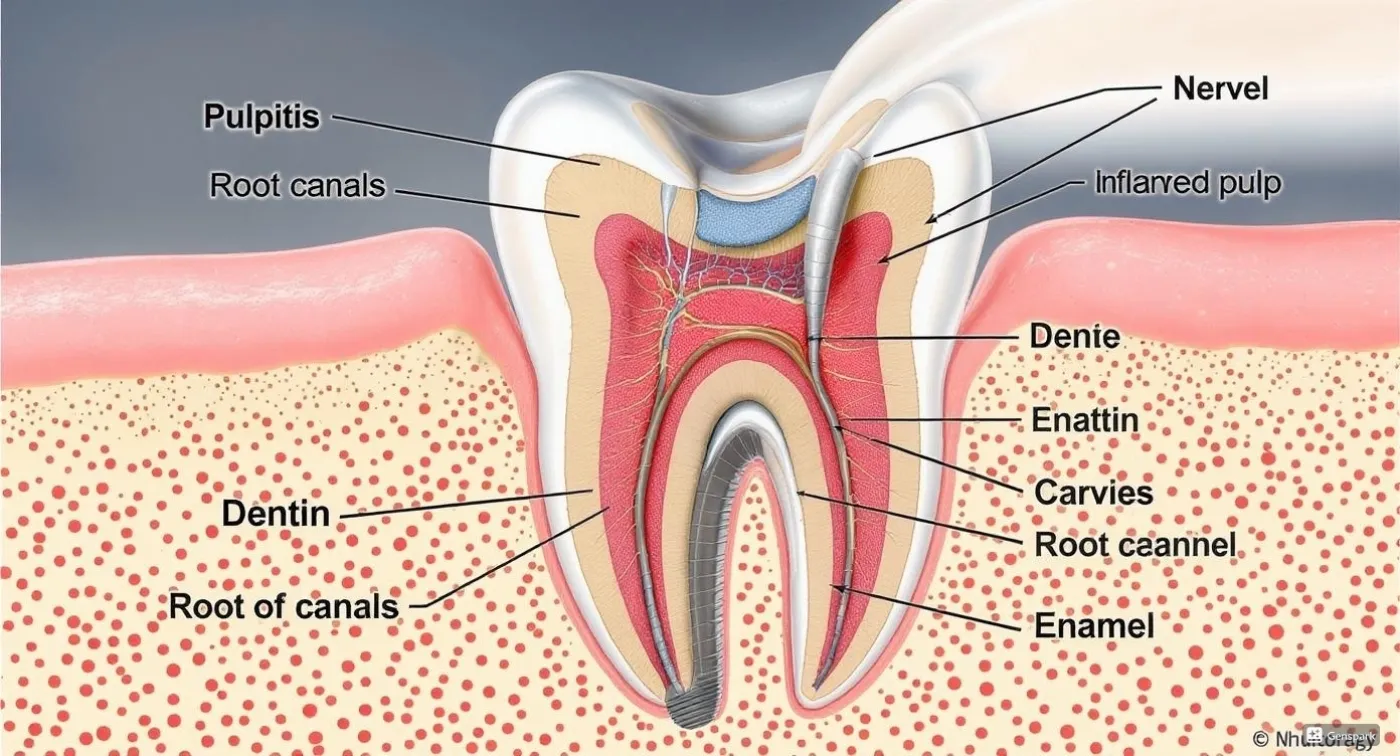
Periodontitis is an inflammatory disease of the periodontal tissues — the structures that surround and support the tooth in the jaw. These include the periodontal ligament, connective tissue, and bone. As the inflammation progresses, these tissues begin to deteriorate. A purulent abscess or even a cyst may form at the tip of the tooth root.
Periodontitis often results from other dental issues, particularly untreated pulpitis (inflammation of the dental nerve). While pulpitis affects the internal part of the tooth, periodontitis develops outside the root, in the surrounding tissues. Unlike cavities, which destroy the hard tissues of the tooth, periodontitis affects deeper structures - bone and ligaments.
On an X-ray, periodontitis typically appears as a dark area around the root, indicating bone tissue damage.
Symptoms of Periodontitis
The symptoms can vary depending on the stage and form of the disease - from mild discomfort to severe pain that disrupts daily activities. Common symptoms include:
- Toothache, especially when chewing
- Swollen, red, or bleeding gums
- A feeling of pressure or heaviness near the affected tooth
- Bad breath or an unpleasant taste in the mouth
In more advanced or purulent cases, general symptoms may appear, such as fatigue, fever, sleep disturbances, swelling of the face or cheek, inflamed lymph nodes, or increased tooth mobility.
If you notice any of these symptoms, it’s time to visit a dental clinic. Periodontitis does not resolve on its own - without proper treatment, the condition will only worsen. The rate at which it progresses depends on your overall health and immune system. Prompt professional care is the key to preventing tooth loss and serious complications.
Causes of Periodontitis
Periodontitis develops due to a number of factors that trigger inflammation at the root of the tooth. The most common causes include:
- Tooth infection. The most frequent cause of periodontitis is advanced tooth decay (caries) that leads to pulpitis and, if left untreated, spreads to the surrounding tissues. The infection can enter through the decayed cavity or, in some cases, from the gum side (retrograde infection).
- Tooth trauma. A cracked root, accidental blows, biting on hard objects, or damage during dental procedures (e.g., improper filling) may cause traumatic periodontitis.
- Failed dental treatment. Low-quality or toxic filling materials, overheating during drilling, or remnants of infected pulp can lead to inflammation of the tooth root area.
Risk Factors:
- Poor oral hygiene. Irregular brushing and lack of professional check-ups increase the likelihood of developing gum and dental diseases.
- Systemic conditions. Diseases like diabetes, cardiovascular issues, gastrointestinal disorders, immune deficiencies, and hormonal imbalances weaken the body’s defenses and increase the risk of inflammation.
- Harmful habits. Smoking, excessive sugar consumption, and an unbalanced diet negatively affect gum and tooth health.
- Childhood. Periodontitis is also common in children. Cavities in baby teeth progress rapidly - it may take only a few months to go from a white spot to pulpitis. Parents should never ignore their child’s complaints of pain or discomfort and should schedule regular dental visits. Inflammation around a baby tooth’s root can damage the developing permanent tooth beneath it.
Understanding the causes and risk factors not only helps in early diagnosis but also plays a key role in preventing complications.
Types and Classification of Periodontitis
Periodontitis is a broad term for various conditions that differ in symptoms, progression, and outcomes. Classification is based on several criteria:
By course:
- Acute. The disease usually begins suddenly and painfully. At first, it may be serous (with slight swelling and moderate pain), but it often quickly turns into a purulent form. Then there is severe, bursting pain, the cheeks swell, lymph nodes enlarge, and the temperature rises. The tooth throbs, becomes mobile, and painful even with light touch. Symptoms of acute periodontitis are a reason to see a dentist as soon as possible.
- Chronic. Often goes almost unnoticed. In this case, the inflammation slowly destroys the tissues around the tooth. Chronic periodontitis may not cause discomfort for years, until a cyst appears or the tooth becomes nonviable. In some cases, the disease may worsen. Then symptoms similar to those of acute periodontitis appear. The chronic form is divided into several subtypes: fibrous, which is detected only on X-ray; granulomatous, where fistulas often form; and granulomatous (a capsule with pus — a cyst or granuloma — forms in the tissues).
By location:
- Apical. The inflammation is located at the tip of the tooth root. Most often occurs due to an infection that has penetrated the root canals.
- Marginal. The inflammation is localised closer to the gums, at the marginal part of the tooth. This form is less common.
By cause:
- Infectious. This is the most common type. The pathogens can be microbes that have entered from a carious cavity or from surrounding infected organs (sinusitis, rhinitis).
- Traumatic. Develops as a result of mechanical impact on the tissues of the jaw.
- Medication-induced (allergic). Occurs as a reaction to aggressive substances used in dentistry, such as iodine or formalin.
Any form of periodontitis requires professional intervention. Depending on the diagnosis, the doctor will prescribe treatment.
Diagnostics of Periodontitis
To diagnose periodontitis, a dentist may use various methods:
- Clinical examination. During the initial consultation, the dentist assesses the condition of the gums, tooth mobility, reaction to percussion (tapping), and sensitivity when biting. The presence or absence of swelling is also noted. Attention is paid to bad breath and the presence of fistulas or purulent discharge.
- X-ray imaging. One of the most informative methods. It allows the dentist to see changes in the bone tissue around the tooth root, the presence of inflammation, granulomas, or cysts. It is often used when a chronic form of the disease is suspected.
- Measuring the depth of periodontal pockets. For this, the dentist uses a special probe. These actions help assess how deeply the inflammatory process has penetrated the tissues.
Early diagnosis makes it possible to stop the development of the pathology, avoid surgical intervention, and preserve the tooth. Therefore, it is important to undergo regular dental check-ups.
Treatment of Periodontitis
Treatment of periodontitis is a set of measures aimed at eliminating infection, reducing inflammation, and preserving the tooth. The therapeutic approach depends on the form of the disease, its stage, and the patient's overall condition.
Conservative Treatment
The first step in therapy is the removal of infected tissue, ensuring pus drainage (in purulent forms), and antibacterial therapy. Treatment of acute purulent periodontitis requires immediate intervention. It includes the following procedures:
- Opening of the root canal;
- Cleaning and antiseptic treatment of infected tissues;
- Application of a periodontal dressing - ensures pus drainage;
- Use of antibacterial medications and rinses - during the time the cavity remains open;
- Canal treatment and placement of a temporary filling — after 3-5 days;
- Monitoring with an X-ray - after a few weeks or months;
- Placement of a permanent filling - if treatment progress is positive.
Therapy for chronic granulomatous periodontitis involves deep cleaning of the canals, prolonged use of medications (from 3 months to six months), and stimulation of tissue regeneration. In the granulomatous form, treatment time may be even longer.
Surgical Treatment
Conservative therapy is effective in 70–90% of cases. However, if it does not bring results or the clinical situation is complex, surgical dentistry methods may be used. This may include, for example, root apex resection or cyst removal.
If the tooth is decaying, severely damaged, or inflammation has spread from the root tip to other tissues, it may not be possible to save it. Conservative treatment may also be impossible due to poor root canal passability. Extraction is the most radical option and is used when preserving the tooth is impractical or impossible.
Prevention of Periodontitis
Periodontitis is a disease that is easier to prevent than to treat. The best protection is responsible daily oral care. To minimise the risks, it is important to follow these recommendations:
- Brush your teeth twice a day. Use a quality toothpaste, a good toothbrush, and the correct brushing technique. It is important to clean not only the teeth but also the tongue.
- Use dental floss or interdental brushes. They help remove food particles from between the teeth, where a toothbrush cannot reach.
- Rinse your mouth regularly with mouthwash. Products with antiseptic properties help maintain a healthy oral microbiome. Rinsing should be done after using floss and after every meal.
Even the most thorough at-home care cannot replace professional dental hygiene. To remove pathogenic microflora, which often accumulates in tartar, it is important to have regular professional cleanings. These can be combined with preventive check-ups. You should visit the dentist at least twice a year. This helps detect problems at early stages and take timely action. If caries, pulpitis, or other dental issues occur, they should be treated as soon as possible.
A healthy lifestyle also plays a crucial role in the condition of your teeth and gums. A balanced diet, avoiding bad habits, and reducing stress are key factors for maintaining good oral health.
Frequently Asked Questions
What tissue forms the periodontium?
The periodontium is made up of connective tissue located in the slit-like space between the cementum of the tooth root and the inner surface of the alveolus.
How long does a tooth hurt with periodontitis?
The duration of pain depends on the type of inflammation. In the acute stage, the pain is usually intense and may last from several days to a week. With proper treatment, it gradually subsides. In the case of chronic periodontitis, the pain is less pronounced and can be described as discomfort during chewing. If chronic periodontitis flares up, unpleasant sensations may persist for several weeks.
What can I use to rinse my mouth with periodontitis?
Mouth rinsing with periodontitis helps reduce tooth inflammation, eliminate bacteria, and speed up the healing process. Dentists most often recommend antiseptic or anti-inflammatory solutions, as well as a baking soda and salt solution. These remedies complement the main treatment and relieve unpleasant symptoms. The dentist will prescribe specific rinsing solutions after an examination and diagnosis.
Can a tooth be saved with periodontitis?
Yes, a tooth can often be saved. The main conditions for this are early detection of periodontitis and timely initiation of treatment. Modern therapeutic methods allow inflammation to be eliminated and tissues around the tooth root to be restored without extraction. The key is not to delay the visit to the dentist.
Conclusion
Periodontitis is a serious dental disease that should not be ignored. Early detection, proper treatment, and a responsible approach to oral hygiene can help avoid complications and keep your teeth healthy. Modern dentistry offers effective treatment methods, including thorough root canal cleaning and tooth restoration. The best way to prevent periodontitis is timely treatment of tooth dacey and regular dental check-ups for preventive care.
Request a call
We will contact you to schedule a convenient time for your consultation and connect you with the right specialist
More articles
We have gathered all the most interesting posts from our specialist doctors in our blog just for you
Dental Treatment During Pregnancy: Myths and Facts

Bruxism (Teeth Grinding) and How to Get Rid of It Forever

Request a call
We’ll get back to you shortly!

Leave a Review
Your feedback means a lot to us!